How To Help Cats In Pain

Do you know when your cat is in pain? You might be able to recognize some obvious signs of pain, like, if you touch an area on the body and the cat re-acts with a hiss or a sudden retraction. But even then you may not be so sure. Could you recognize the not-so-obvious signs of pain? Maybe not.
There are challenges in treating feline pain. First, because cats have an unique metabolism there’s not that many prescription drugs labeled for cats. Cats lack a liver enzyme called glucuronyl transferase which is responsible for changing some hormones, medicines, and toxins into non-harmful products. This makes cats very susceptible to all types of toxicity, such as, plants containing phytoalexins, NSAIDs, chocolate, caffeine, lead, zinc, pesticides, etc. If we do manage to find a medication to give to cats most cat owners will tell you how difficult it is to pill a cat.
Another thing I have found is a lack of information on how to deal with pain in cats. I may find a few published peer-reviewed studies on dogs and it may suggest applying it to cats, but cats aren’t dogs. And, cats express pain differently than dogs. Plus, there is a good possibility cats will react adversely to canine prescribed meds.
This may be hard to believe, but at one time veterinary scientists didn’t think animals experienced pain. It took until 1987 for the American Veterinary Medical Association to recognize and assess pain in animals or even to provide alleviation for such pain. Before that they only acknowledged that animals showed the physiological correlations of pain, such as nerve impulses, changes in hormonal levels, and reduced movement. But because they were afraid of being accused of anthropomorphism, scientists refused to believe animals responded emotionally to pain the way humans do.
In the wild, it would make sense an animal would hide their injuries so not to alert their predators. Any sign of weakness could mean death. As Cindy Engel writes in her book Wild Health, “To survive, an animal must not only be healthy, but must look healthy.”
Cats Are Good At Hiding Pain
So, how do we recognize pain in cats? One way could be a change in normal behavior. For example, your cat used to jump up on the counter as you prepared lunch. But now, he doesn’t do that anymore. It may mean the cat has arthritis and it hurts to jump. Or, there may be a new or strange behavior. For example, my sister had a Japanese Bobcat that suddenly became very hostile to the other cats in the house. The cat would isolate herself on top of the kitchen counter and if you walked anywhere near her she would hiss and lash out. These were all new and odd behaviors. It turned out the cat had cancer. Obviously, she must have been in a lot of pain.
Other signs is a change in grooming. The cat has stopped grooming and the fur has become matted. Or, he is now over grooming, or is fixated on one area. Or, a cat would go off somewhere and hide, often times in very unusual places. Also, look out for excessive tail activity, decreased appetite, vocalization, contractions and extensions of the hindlegs, partially closed eyes, reaction to palpation of the abdomen and flank.
The Feline Grimace Scale
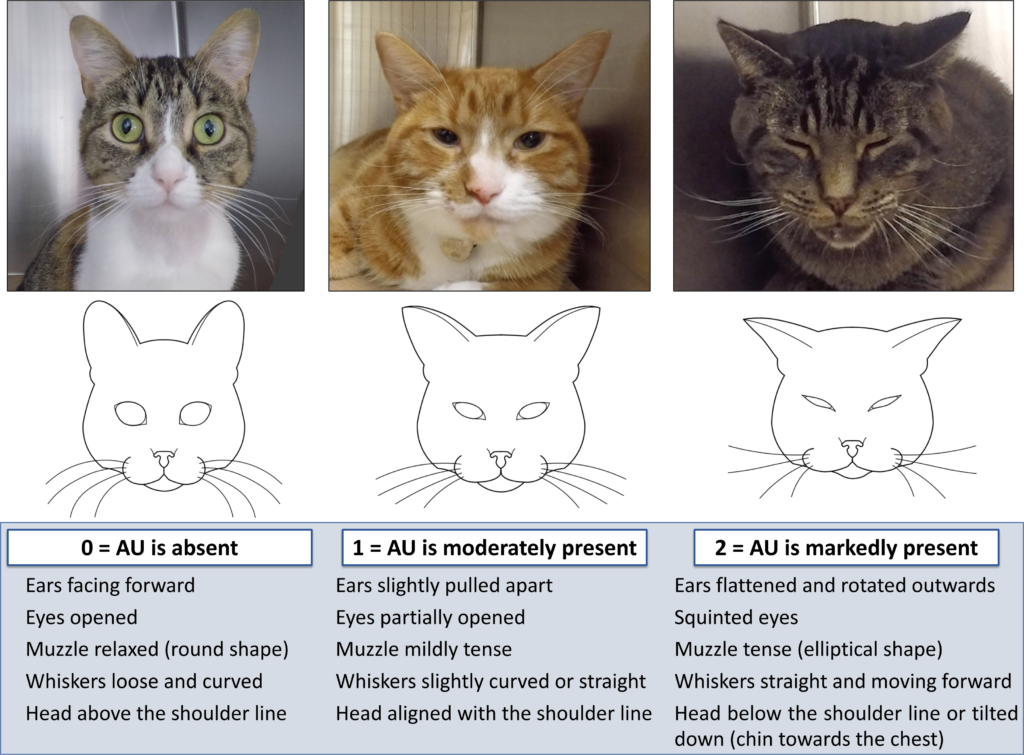
Something else cat owners may want to pay attention to is the Feline Grimace Scale. This tool is from the University of Montreal. It is a simple method of pain assessment using changes in facial expressions. The researchers used video recordings of 70 cats and compared images of painful and non-painful cats. They found that the position of the eyes, ears, whiskers, muzzle and head changes under painful conditions. These changes will return to their normal position after the cats were given pain killers. Tests show the scale is accurate, valid and reliable. And this helped to give a cut-off score for rescue analgesia.
There are other Pain Scales that can be used to evaluate pain in cats. Such as, The Feline Musculosketel Index which is often used for scaling degenerative joint disease (DJD). And, together with the Grimace Scale, there is the Colorado Acute Pain Scale that post illustrations to rate a cat’s pain, especially after surgery.
Joint Pain In Cats
Osteoarthritis is the leading cause of chronic pain and lameness in cats, and dogs, too. Studies have shown, 20% of dogs and 22% of cats show radiographic evidence of osteoarthritis before the age of two-years old. In cats 12-years old and older, 90% had radiographic signs of osteroarthritis, and of that age group, only 16.5% displayed clinical signs of lamesness. So, by the time your cat is 12-years old there’s a good chance it may have arthritis and you wouldn’t know it.
Osteoarthritis is often treated with NSAIDs. Unfortunately, besides the side effects of vomiting, diarrhea, GI ulcers and GI perforation, NSAIDs can actually accerlate articular cartilage degeneration.
The studies I’ve read on feline osteoarthritis say things like “they don’t know why cats develop osteoarthritis,” especially at younger ages. They speculate it could be from old injuries, obesity, genetics. But two things they don’t mention are: at what age the cats in the studies were neutered or spayed, or what were the diets of these animals. Well, I have my own suspicions of other contributing factors:
In the US, it is very common to spay and neuter our cats and dogs while they are still juveniles. The sex hormones are responsible for regulating bone growth. So, when the ovaries and testes are removed, the growth hormone can not be properly controlled. As a result, the bones grow longer than they ought to be. Normally, the growth plates, or the epiphyseal plates, would close when the animal reaches maturity at around 18 months to 24 months of age. But, when the sex hormones are removed, let’s say, at 3 months of age, the closure of the bone plates are delayed leaving the animal vulernable to injuries.
Some veterinary surgeons have also raised the possibility that early neutering may lead to a higher incidence of physeal fractures because of a delay in growth plate closure (Spain et al, 2004). A study by Root Kustritz et al (1997) showed that early neutering does lead to a delay in growth plate closure, and therefore the long bone growth may be slightly increased. McNicholas et al (2002) monitored cats presented with capital physeal fractures (mean age 22 months), and found that 25 out of 26 of these cats were neutered males.
In studies on the health affects of desexing in large breed dogs, it has shown an increase in the chance of hip dysplasia, and cranial cruciate ligament (CCL) ruptures, a degenerative joint disease. You can read the Study here.
New research involving a large sample of dogs revealed older age, higher adult body weight, gonadectomy, and younger age at gonadectomy were significantly associated with higher risks of osteoarthritis in the total cohort and in all 12 breeds evaluated. Read Study.
Another thing I suspect is the diet. Were all the cats in the study fed a commercial ultra-processed pet food? Did the diet include kibbles? This is important because ultra-processed food and carbohydrates can cause insulin resistance which triggers chronic low-level inflammation throughout the body. Thus, this can lead to inflammatory diseases, like, dermatitis, pancreatitis, arthritis, cancer, diabetes, etc. On top of that, processed pet food contain an imbalance of essential fatty acids. Cats and dogs can’t produce essential omega-3 (DHA) and essential omega-6 (LA) on their own and must get it from their diet. Ultra-processed commercial pet food are not required to contain Omega-3s. Foods like kibble can be 30% to 60% Omega-6s, and with an imbalance like this inflammation can surely set in.
A 2022 study from Canada, wanted to test the analgesic effects of fortified food and nutraceuticals given to cats and dogs suffering from osteoarthritis. The study found that Omega-3 enriched diets had an evident clinical analgesic efficacy, including Omega-3 supplements combined with cannabidiol (to a lesser degree). The study also showed a weak efficacy of collagen, and that chondroitin-glucosamine nutraceuticals had a very marked non-effect. As a result, chondroitin-glucosamine is no longer recommended for pain management in osteoarthritis for cats and dogs (Please read the STUDY).
How To Treat Pain In Cats
Once we’ve figured out our cat is in pain, what can we do?
Because I am an Animal Naturopath I am a drug-less practitioner. Later on, I’ll discuss some drugs that are commonly used in veterinary medicine, but first let’s talk about natural remedies.
Homeopathy:
When my Siamese cat, Mali, turned 20-months old, I decided to have her spayed. After the surgery, I picked her up at the vet. I was surprised they didn’t hand me any pain killers. The vet tech told me my cat didn’t need them. I said, “Mali just had surgery. She was cut opened and had an organ removed and you’re telling me she doesn’t need pain killers?”
“No,” said the vet tech. “She’ll feel out-of-it for the first 24 hours. She’ll probably won’t want to eat. But the next day, she’ll be fine like nothing even happened.”
Well, that’s not true. I could see when I brought her home that she was miserable. Her Grimace Scale was AU-1. To help alleviate her pain I administered homeopathic remedies, like, Bellis Perennis, and a few other remedies to give her some pain relief (please see my blog Pain Management Using Homeopathy).
If you read my blog Is There Evidence Homeopathy Works For Animals you’d see I posted one study that looked at alleviating pain and distress in tail-docking in lambs. Researchers found a combination of homeopathic remedies of Aconite, Arnica, and Hypericum reduced pain by 30%.
Why were those remedies chosen? Arnica is a well-known remedy used for traumatic injuries to muscles, concussions (head trauma), compound fractures, bruises, pain from physical shock, sprains, etc. Hypericum is used for any damage or injury to the nerves, wounds or injuries that feel worse from touch or pressure, pain from puncture wounds, etc. Aconite is a remedy for the effects of anxiety, shock, or fear, which I’m sure the lambs felt from the tail-docking.
Other homeopathic remedies for pain:
Rhus Tox – affects skin, mucus membrane, fibrous tissues, ruptured ligaments and tendons of muscles around joints. Arthritis and similar conditions. Bruises from blows or falls. Lamesness, stiffness, pain on first moving but relieved by continuing motion. Restlessness from pain, must keep moving.
Ruta – Like Arnica, also acts on bruised muscles, torn tendons, spilt ligaments of joints. Knee, wrist, and elbow injuries; shin injury and shin splints. Pain after osteopathic manipulations of the spine and pelvis.
Symphytum – Acts on the periosteum and the bones. If Ruta should fail to relieve periosteal pain within 24 hours, go to Symphytum which has a deeper action. It hastens the formation of callus, which is necessary for the repair of bones.
Bellis Perennis – For the effects of major physical trauma to deeper tissues; after major surgery. Trauma to pelvic organs (abdominal wall and uterus) with sore bruised feeling; pains of childbirth.
There are more homeopathic remedies to help alleviate pain, but I’ve only named a few. The remedies I listed are the most common. You can always book a consultation with me if you have any particular need.
Acupuncture
Not too long ago, I had chronic neck pain that was so severe I could barely function throughout my day. I tried everything from deep massage to seeing a chiropractor but nothing worked. That is, until I saw an acupuncturist. After only 3 acupuncture sessions I was finally pain free.
If acupuncture worked for me can it work for animals? A newly published article, ‘Evidence-Based Application of Acupuncture for Pain Management in Companion Animal Medicine’, explores the evidence base for the use of acupuncture as a medically appropriate, scientifically driven treatment for pain in companion animals.
Supplements:
Omega-3s:
Omega-3 is made up of two essential fatty acids, DHA and EPA. It can be found in organ meats and fish. It helps to decrease pain and improve weight-bearing. Fish oil Omega-3s decreases prostaglandins. Prostaglandins are the substance that cause joint inflammations.
Green Lipped Mussel
Green lipped mussel contains GAGs (glycosaminoglcans) which include natural substances like hyaluronic acid, glucosamine or chondroitin. These have all been shown to lubricate the joints and support connective tissue like cartilage and tendons. It is especially rich in chondroitin sulfate, which can help build healthy cartilage. But, as I mentioned above, a Canadian study of glucosamine and chondroition did not show to be effective in pain management.
Green lipped mussel is rich in an unique Omega-3 fatty acid called Eicosatetraenoic Acid (ETA).
Usually, it takes two weeks to see results, and even better results after 12 weeks.
Turmeric
Turmeric (Curcumin longa) is a common spice in many kitchens. It has anti-inflammatory properties and may be helpful in arthritis, heart disease, inflammatory bowel disease, cancer, diabetes, and as a paste for wound healing. The powder can be easily mixed in food.
Boswellia
Boswellia, also known as frankincense, is from the resin of the boswellia serata tree. It is effective for osteoarthritis, rehumatoid arthritis, asthma, Inflammatory Bowel Disease, and it helps prevent cartilage loss. Boswellic acid blocks the pro-inflammatory enzyme 5-lipoxgenase which inhibits the synthesis of leukotrienes.
If you do choose to give your cat Boswellia, just remember, it has a horrible taste. So, it’s best to administer boswellia in pills (if you can successfully pill your cat).
CBD Oil
Humans and animals alike all have an endocannabinoid system (ECS). When CBD oil is consumed, it activates your dog or cat’s ECS. The ECS then creates a two-way communication system between the brain and other systems in your pet’s body, such as the nervous system, immune system, digestive system, and more.
The clinical application of CBD is for pain, both acute and chronic. There is some thought for use in epilepsy, as it can attenuate seizures. CBD is neuroprotective, which makes it act like an antioxidant. Also, it helps to reduce the development of mellitus diabetes in diabetic prone mice and reduce pancreatic inflammation. For bone formation, CBD stimulates stem cells responsible for fracture healing. For cancer, it has shown anti-apoptotic effects and reduce tumour proliferation—and anecdotal reports of remission.
Now that marijuana is legal in many US States, veterinarians are not allowed to prescribe medicinal marijuana to pets. Not yet, anyway. However, your veterinarian is allowed to prescribe CBD oil.
I’d like to caution pet owners from giving their cats or dogs marijuana because they are extremely sensitive to the THC in marijuana. Instead, use Hemp oil products as they are high in CBD and other non-psychotropic cannabinoids (such as terpenes and terpenoids) and low in THC.
CBD from Hemp or a purified source of CBD should be used.
Traditional Chinese Medicine For Pain
From a Traditional Chinese Medicine perspective there are two conditions of pain. The first is called Full Condition and the second is Empty Condition.
Full Conditions: Invasion of Exterior Pathogens; Interior Cold or Heat; Stagnation of Qi or Blood; Retention of Food; Obstruction of phlegm.
Empty Conditions: Deficiency of Qi or Blood; Consumption of Body Fluids from Yin Deficiency.
Chronic illnesses are mostly Empty Conditions, and Yin Deficiences are more common in our older pets. In chronic pain, you often have Qi stagnation and Blood stasis. So, as long as Qi and Blood flow freely, there is no pain.
In Qi stagnation, there will be a distention of pain with no fixed location. Oftentimes, this pain comes and goes. Qi stagnation can occur in the channels or in the lower jiao (liver, stomach, intestines). Think of cats with pancreatitis, vomiting. Also, excess activity or inactivity (lack of exercise) can lead to Qi stagnation.
If the Qi is stagnant too long then it can lead to Blood stagnation, or Blood stasis. Also, excess Cold or Heat, Deficient Qi or Blood, as well as, a build up of Phlegm can all cause Blood stasis. The Blood stasis pain is often severe or stabbing and tends to be fixed in one location. In these cases, it is important to improve circulation. And, this is where herbal remedies and acupuncture can be used to move the Blood and Qi.
So, how do we know whether we’re dealing with Full or Empty Conditions? First, we can scan acupuncture points to see where the blockage is, exam the animal’s health history, and take a look at the pulse and tongue diagnosis.
Pulse Electromagnetic Therapy
When I think of PEMF therapy, I think of the Assisi Loop. As described on their website:
Targeted Pulsed Electromagnetic Field (tPEMF™) therapy delivers a micro-current to damaged tissue that is precisely tuned to trigger an animal’s own natural anti-inflammatory process. The electromagnetic signal stimulates cellular repair by upregulating the body’s own production of endogenous nitric oxide (NO).
The magnetic pulse does not create heat. It directly alters cellular signaling. So, basically it targets the mitochondria. The tissues that PEMF tends to affect, are blood, muscles, ligaments, and cartilage. That’s because these tissues respond to biophysical input, including electrical and electromagnetic fields.
PEMF can reduce pain and inflammation, increase healing time, increase bone mineral density (for those bones that don’t heal), and reduce tissue necrosis.
Cold Laser Therapy/Red Light Therapy
Cold laser therapy can speed up healing and reduce pain by stimulating the tissues at a cellular level. The treatment is safe and effective for both small and large animals.
P.E.A. (Palmitoylethanolamide)
Palmitoylethanolamide, aka PEA, is a naturally occuring amino acid compound found in plants and animals.










